Healthcare payment systems can feel a bit like deciding between paying for each item on a menu or going for a buffet. Fee-for-service (FFS) charges you for every test, treatment, or visit separately, which can add up quickly. Value-based care (VBC) works differently. It focuses on keeping patients healthier overall, with providers rewarded for better outcomes instead of how many services they provide. Knowing the difference helps patients and providers make smarter choices about care and costs. Let’s learn more about value-based care vs fee-for-service models.
Understanding Fee-for-Service (FFS)
The fee-for-service model in healthcare pays providers for every service they deliver. This includes every test, treatment, consultation, or procedure, regardless of its outcome or necessity. While it may seem straightforward, this payment structure prioritizes quantity over quality. Providers are paid more the more services they provide, which can unintentionally create an environment where efficiency and effectiveness take a backseat to volume.
Fee-for-service has faced criticism for potentially leading to overutilization of services. With no direct link between payment and patient outcomes, the model may encourage unnecessary tests or treatments, increasing healthcare costs without guaranteeing better care. Critics argue that this approach doesn’t incentivize preventative care or long-term health improvements, leaving patients with fragmented care rather than coordinated treatment focused on well-being.
Understanding Value-based care (VBC)
Value-based care focuses on improving patient health outcomes rather than the volume of services provided. Under this model, healthcare providers are reimbursed based on the quality of care they deliver. The emphasis shifts to preventing illness, managing chronic conditions, and ensuring patients achieve healthier results. This approach improves the patient experience and encourages providers to focus on long-term well-being instead of short-term interventions.
The Centers for Medicare and Medicaid Services (CMS) have set clear goals to expand value-based care, especially among Medicare beneficiaries. By prioritizing quality over quantity, this model aims to reduce unnecessary procedures and lower healthcare costs while improving access to care. Patients benefit from a more personalized approach to therapy, while providers benefit from increased innovation in offering effective care solutions.
Let's give you a clear comparison of Value-based Care vs Fee-for-Service models.
Related Read: The Road to Value-based Healthcare: How Interoperability Paves the Way
Value-Based Care vs Fee-for-Service: A Clear Comparison
🏁 Outcomes and Quality of Care
Fee-for-service focuses on the volume of provided service, meaning healthcare providers earn based on the number of procedures, tests, or visits. Value-based care focuses on the quality of results. Providers are rewarded for helping patients achieve better health through efficient treatments and preventative care, shifting attention from quantity to long-term results.
💰 Reimbursement and Financial Risk
In fee-for-service, providers earn for each service, regardless of patient outcomes, leaving little financial risk for the provider. Value-based care shifts financial incentives by linking reimbursement to performance and patient results. This model often involves shared financial risk, where providers may incur costs for poor outcomes and gain rewards for improving patient health.
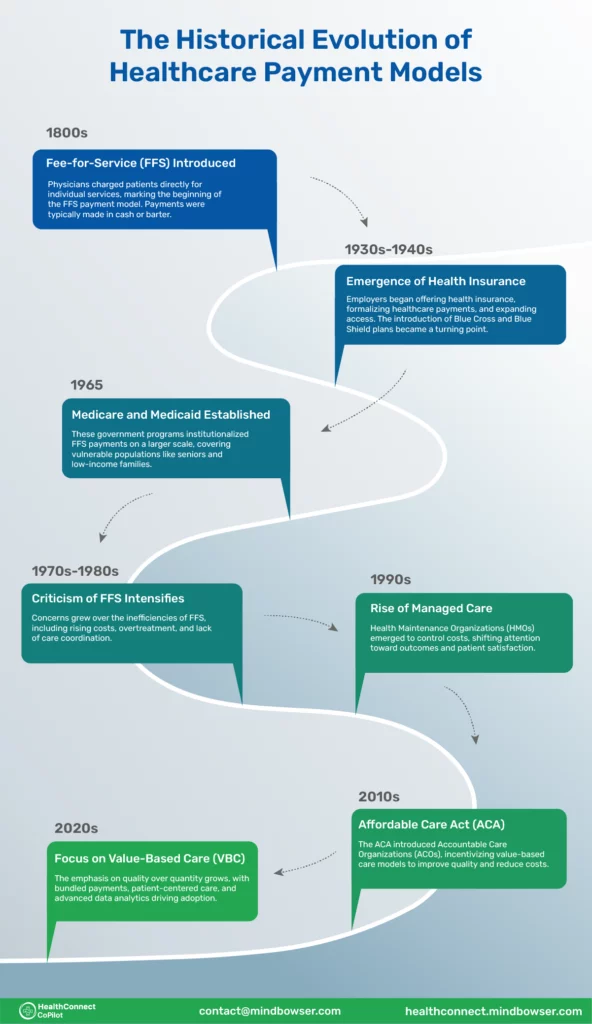
🔁 Transition to Value-Based Payment Models
Healthcare systems are increasingly adopting value-based care to address inefficiencies in fee-for-service. This transition focuses on improving outcomes, reducing unnecessary services, and controlling costs. Government programs, insurers, and providers are gradually moving to value-based care arrangements to prioritize patient well-being and sustainable healthcare spending.
🤑 Financial Incentives and Out-of-Pocket Costs
Fee-for-service can lead to higher patient costs due to its focus on delivering more services. Value-based care, on the other hand, promotes cost-effective care by incentivizing providers to focus on preventive care and efficient treatments. For patients, this can result in lower out-of-pocket expenses and fewer unnecessary procedures.
📃 Claims and Forms
Administrative processes differ significantly between the two models. fee-for-service typically involves more claims and paperwork for every individual service, leading to a complex billing system. Value-based care streamlines administrative efforts by bundling payments for entire episodes of care or offering fixed reimbursements, reducing the administrative burden on providers and patients alike.
🏥 Accountable Care Organizations (ACOs)
Accountable care organizations are important in advancing value-based care by coordinating care among multiple providers. They aim to deliver high-quality care while managing costs effectively. Under value-based care, accountable care organizations ensure patients receive the right care at the right time, avoiding unnecessary duplication of services and minimizing medical errors.
How HealthConnect CoPilot can help you with the transition from Fee-for-Service to Value-Based Care?
The shift from fee-for-service to value-based care represents a major change in healthcare. Fee-for-service focuses on quantity; providers are paid for every service, test, or procedure performed, often leading to fragmented care. Value-based care emphasizes quality, rewarding providers for improving patient outcomes while reducing costs.
Transitioning to value-based care can be challenging. Providers must adopt new workflows, integrate advanced technologies, and track patient data effectively to meet outcome-based goals. Resistance to change, financial risks, and complex data requirements can complicate the process.
HealthConnect CoPilot supports healthcare organizations during this transition by offering solutions that streamline workflows, integrate data from various systems, and provide tools to measure and track patient outcomes. With expertise in health tech and interoperability, We simplify the move to value-based care, ensuring providers stay focused on delivering quality care while adapting to new models.
- What is the main difference between value-based care and fee-for-service?
Fee-for-service focuses on the volume of services provided, where healthcare providers are paid for each procedure, test, or consultation. Value-based care, on the other hand, emphasizes quality and outcomes, rewarding providers for delivering effective and efficient care that improves patient health.
- How does value-based care improve patient outcomes?
Value-based care encourages healthcare providers to focus on preventive care, patient education, and coordinated treatment plans. By addressing root causes and avoiding unnecessary procedures, it helps improve overall patient health and reduces complications.
- Why might providers prefer fee-for-service?
Fee-for-service offers providers greater control over their treatment decisions and guarantees payment for each service performed. It can be financially rewarding, especially in high-volume practices, and does not require the extensive data tracking associated with value-based models.
- What are the challenges of transitioning to value-based care?
Switching to value-based care involves adopting new technologies, changing workflows, and meeting specific performance metrics. Providers may face financial uncertainty during the transition, as compensation becomes linked to patient outcomes rather than service volume.
- How can healthcare organizations navigate the shift from fee-for-service to value-based care?
Organizations can prepare by investing in data-driven technologies, training staff on performance-based care, and collaborating with experienced partners to streamline the transition. Support from consultants and tech solutions can help providers adapt to new models without compromising care quality.

Pravin Uttarwar, CTO of Mindbowser
As the CTO of Mindbowser, a healthcare-focused software development company, I am dedicated to delivering cutting-edge digital solutions that transform patient care and operational efficiency. With over 16 years of experience and as an MIT alumnus, I specialize in healthcare interoperability, FHIR-compliant systems, and AI-powered platforms, crafting scalable products and architectures tailored to the unique needs of healthcare providers and enterprises.
I have spearheaded the development of over 100 products and platforms, guiding them from concept to full-fledged solutions. My expertise extends to scaling remote tech teams, driving EHR integrations, and building secure, cloud-native healthcare solutions. By shaping technology visions and roadmaps, I help clients achieve long-term growth and success in the rapidly evolving healthcare landscape.
HealthConnect CoPilot enabled us to access real-time patient health data through integration with Apple HealthKit, enhancing care delivery while maintaining HIPAA compliance. This led to personalized care and improved outcomes for patients.
AI-enhanced Obstetrics Clinical Decision Support Platform
HealthConnect CoPilot's integration with Epic's Hyperspace has transformed our workflow. Automated post-delivery examinations and HL7 protocol use ensure accurate updates to Epic. Their expertise empowers informed decision-making in childbirth

Top Provider for Customized Healthcare Solutions
HealthConnect CoPilot's helped us to integrate with leading tracking devices such as Apple Watches and Fitbit. This integration enables effortless syncing of health data, providing users with real-time insights displayed directly on our flagship products: smart mirrors and digital calendars.

A Provider of Customizable Display Solutions
Post a comment Cancel reply
Related Posts
Navigating the Future of Healthcare Integration with SMART on FHIR Apps
SMART on FHIR enables apps to plug directly into EHR systems like Epic EHR, Cerner…
TEFCA in Healthcare: A Complete Guide
Healthcare has long struggled with fragmented data systems. Patient records are often locked within isolated…
Model Context Protocol (MCP): Revolutionizing Healthcare Chatbots with FHIR Integration
Healthcare technology is experiencing a paradigm shift with the emergence of Anthropic’s Model Context Protocol…
Healthcare Integration: The Understanding & Its Impact in Healthcare
Healthcare integration refers to connecting various systems, applications, and data sources within the healthcare ecosystem…
Checklist for EHR Integration in the Healthcare System
EHR integration in the healthcare system refers to the seamless connection of EHR systems with…
Integrating FHIR and Genomics: How AI is Shaping the Future of Medicine
AI is transforming the way medicine approaches personalized healthcare, particularly through genomics. By analyzing vast…









